Introduction: Why the Adriana Smith Case Matters
The Adriana Smith case is not just a tragic personal story, it’s a mirror reflecting the unresolved tension between law, medicine, and ethics in reproductive care.In December 2024, Adriana Smith, a 26-year-old pregnant woman and mother of two, suffered a massive stroke in Georgia. She was declared brain-dead soon after. But for over four months, her body remained on life support.
Why? Because her fetus had a heartbeat, and under Georgia’s LIFE Act, that was enough to override her family’s wishes and delay end of life decisions.
This case forces us to confront difficult questions: How should hospitals balance medical ethics and evolving abortion laws? Can a fetus’s legal rights outweigh the dignity and consent of a brain-dead woman? What happens when fear of litigation replaces compassion?
Timeline of Events
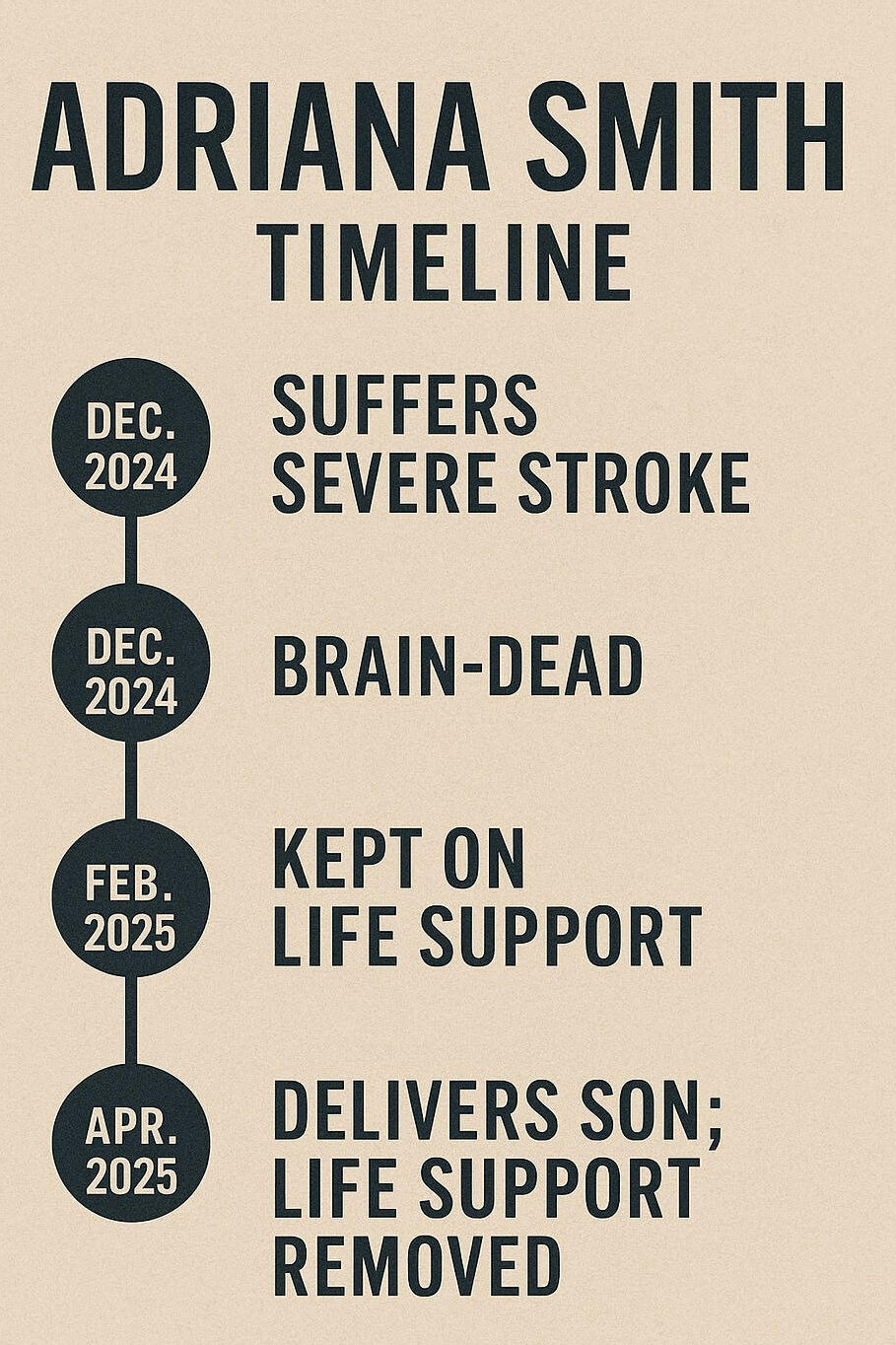
The story of Adriana Smith unfolded over four agonizing months, each moment underscoring a growing disconnect between law, medicine, and family agency.In December 2024, Adriana arrived at Emory Hospital in Georgia after suffering a severe stroke. She was 13 weeks pregnant. Despite attempts at medical intervention, she was declared brain-dead within days.Legally, this should have marked the end of life, but because her fetus still had a detectable heartbeat, the hospital refused to remove her from life support.
From late December through April 2025, Smith’s body remained artificially sustained in a state of biological suspension.Her family, who pleaded for her prior wishes to be honored, were told the hospital could not legally act until the fetus was viable or delivered.This decision was justified through Georgia’s LIFE Act, which grants legal rights to a fetus once a heartbeat is detected, but the law itself does not clearly outline procedures for cases involving brain-dead patients.
Medical and Ethical Breakdown
The ethical crisis in the Adriana Smith case began when Emory Hospital claimed it had to comply with the Georgia LIFE Act. This law grants fetal constitutional rights once a heartbeat is detected, typically at six weeks.
Though brain death is considered legal death in Georgia, the hospital interpreted the LIFE Act to mean that terminating life support could be legally risky, even though the law did not mandate this action.
Ethical Violations:
- Autonomy: Smith’s and her family’s wishes were completely ignored
- Non-maleficence: Prolonged support risked trauma to her deceased body
- Beneficence: No medical benefit existed, only legal defensiveness.
- Justice: The case highlights how women, particularly women of color, face disproportionate denial of dignified care.
Quote from a Legal Scholar
“Adriana Smith’s case is not an abortion story. It is a story about how misapplied law can silence families, paralyze doctors, and strip people of dignity, even in death.”
— Dr. Lena Hastings, Professor of Health Law, Columbia University
What Should Have Happened: Legal and Ethical Response
Despite hospital claims, the Georgia Attorney General’s office later clarified: the LIFE Act does not require life support for brain-dead pregnant patients. Brain death is, and remains, legal death.
So why was Adriana Smith kept on life support?
- Misinterpretation of fetal personhood laws
- Fear of civil or criminal prosecution
- Lack of internal protocols for brain-dead pregnancy
The legally and ethically appropriate steps would have been:
- Confirm brain death as the end of legal personhood
- Allow surrogate family members to make decisions
- Consult hospital ethics board
- Uphold patient dignity
The Fetal Personhood Conflict
The Adriana Smith case highlights a dangerous gap in fetal personhood laws. Over 15 states in the U.S. have recognized fetal legal rights either through heartbeat laws or constitutional amendments. Georgia’s LIFE Act grants such rights after heartbeat detection, around six weeks.
But these laws rarely address nuanced, high-stakes cases like:
- Maternal brain death
- Fetal non-viability
- Conflicting family or surrogate consent
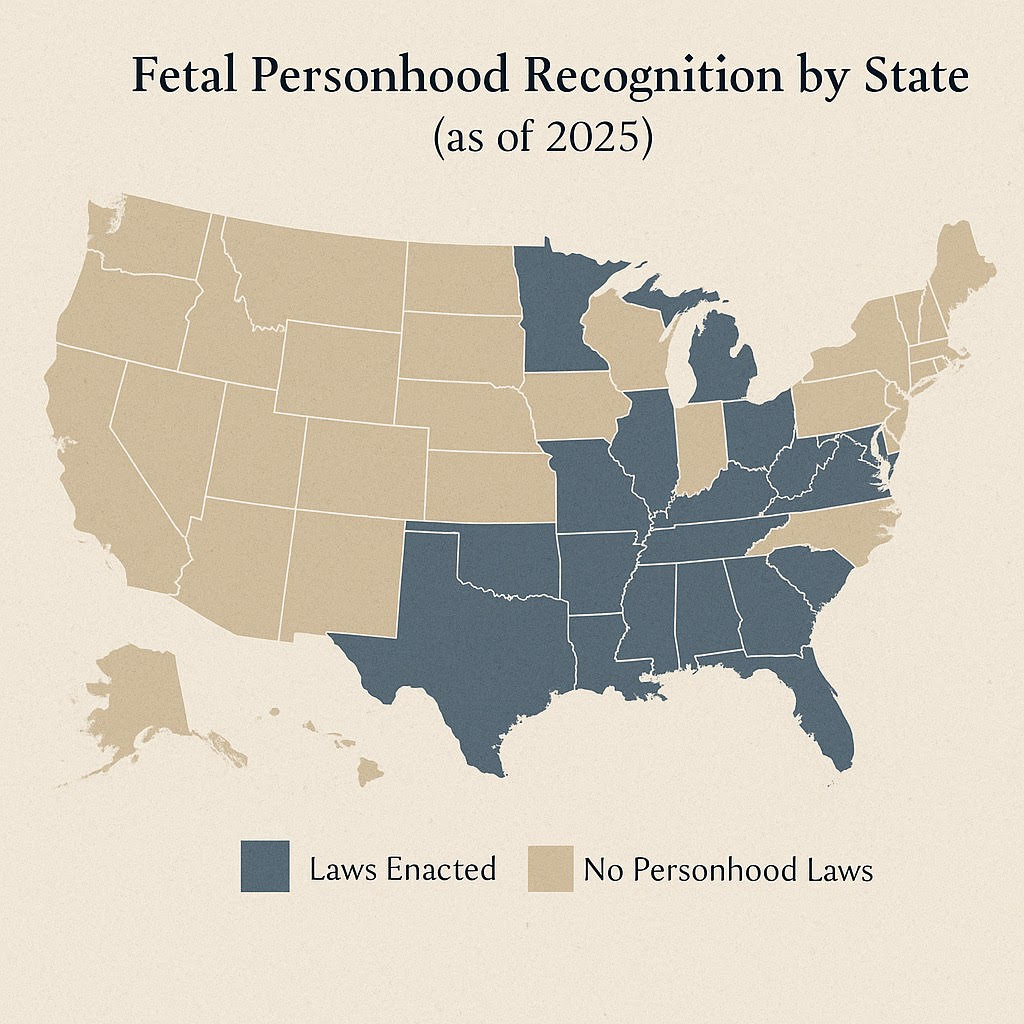
In Adriana Smith’s case, the fetus was just 13 weeks old when she was declared brain dead, not viable by any medical standard. Yet, due to legal ambiguity, her body was kept functioning for months, not for her benefit, but to protect the hospital from potential lawsuits.
Global Comparison of Medical Law
In most countries, this would never have happened. Brain death is legally recognized as the end of life, and fetal personhood is not used to override consent or dignity.

These differences show that the Adriana Smith case is not just a legal tragedy, it’s a failure of legal preparedness in complex medical emergencies.
LexNova Commentary
The Adriana Smith case is what happens when legal ambiguity overrides ethical medicine. It is a wake-up call to rethink fetal personhood frameworks, especially in emergencies where the patient can no longer speak for herself.
When medical teams are forced to prioritize legal protection over patient-centered care, justice fails. Dignity fails. Ethics fail.
LexNova strongly urges policymakers to issue clear, humane guidance for maternal brain-death cases and ensure healthcare law serves the living and the deceased with equal respect.
Policy Recommendations
- Protect advance directives, even during pregnancy
- Explicitly exempt brain-dead patients from fetal personhood statutes
- Establish ethics review protocols in emergency maternal care
- Educate medical staff on legal obligations vs ethical responsibilities
- Center racial and gender equity in reproductive healthcare law
References
Georgia House Bill 481 – Full Text via Legiscan
Washington Post – Brain-dead woman taken off life support after delivering baby
Contact LexNova
Reach out for consultations.
FAQs- Adriana Smith
Is brain death legally considered death in Georgia?
Yes. Georgia recognizes brain death as legal death.
Did the LIFE Act require hospitals to keep Smith on life support?
No. The law was misinterpreted. The Attorney General confirmed it did not mandate this action.
Was Adriana Smith’s fetus viable?
No. At 13 weeks, the fetus was well below the threshold of viability (~23 weeks).
What happened to the baby?
The baby was delivered via C-section and remains under care. The family has requested privacy.
How would this case unfold in other legal systems?
In most jurisdictions, consent and finality of death would be respected over potential fetal rights.
Disclaimer
This blog is intended for informational purposes only and does not constitute legal advice.